REX Awards 2023: Technology and Automation
The shining stars of the technology and automation industry are the companies that are continually innovating and enabling pharmacists to practice at the top of their licenses. They also are increasing efficiencies so that pharmacists are free to provide a myriad of clinical services. During these highly competitive times, they rise to the occasion to give retailers an opportunity to interact with their customers and help patients to lead healthier lives.
In April, Drug Store News recognized the luminaries of the technology and automation industry with its Retail Excellence Awards—Technology and Automation. These are companies that are continually striving to do their best for their customers.
Adheris Health
Woburn, Mass.-based Adheris Health, a MedAdvisor company, has been a pioneer and leader in direct-to-patient engagement in the United States for more than 30 years.
“There is a huge opportunity to improve the estimated $528.4 billion annual cost from non-optimized medication therapy and the loss of over 275,600 lives,” said Jim Rotsart, general manager of U.S. operations at Adheris Health. “This distressing trend is something we are continually committed to turning around by transforming and individualizing medication management to empower people to live healthier. We do this by supporting the patient at every point-of-care, when and how they need it—at the pharmacy, at home with direct mail or virtually with smart digital solutions.”
Adheris Health provides content, education, support and resources to help address the barriers of care, whether it be overcoming lifestyle challenges, a need for understanding proper therapy usage or lack of affordability. The company delivers individualized patient medication experiences to empower patients for a successful treatment journey and improve outcomes for patients, retailers, brands and payers.
“Our retail partnerships and product portfolio continue to expand as we accelerate and solve for even more market challenges, bringing forward solutions that drive more success for our partners and as a result, patients,” Rotsart said.
Adheris Health continues to introduce new and innovative solutions to empower patients further to start and stay on therapy.
“We are laser-focused on launching new, innovative solutions to further bring our vision to life,” Rotsart said, noting that the company’s most recent innovation enables pharmacies to digitally deliver their required regulatory content to patients, including medication guides, product images and drug monographs. Adheris Health plans to expand this solution with additional features to drive additional value for retailers.
CoverMyMeds
Columbus, Ohio-based CoverMyMeds, part of McKesson, is a medication access company committed to helping people get the medicine they need. Created in 2008 to help streamline the traditionally manual prescription prior authorization process, CoverMyMeds has built a robust industry network and technology solutions that help providers and pharmacists better serve their patients.
CoverMyMeds’ solutions help address fundamental barriers to medication access, affordability and adherence. These solutions integrate with pharmacy management systems to help improve workflows, enabling pharmacists to focus more on patient care. CoverMyMeds also offers solutions that help improve pharmacy operations, including electronic prior authorization, claims adjudication, central fill dispensing and medication affordability solutions that help prevent abandonment.
“CoverMyMeds continues to enhance its retail pharmacy solutions, including services that give our customers additional prescription fulfillment flexibility,” said Melanie Christie, vice president of product management at CoverMyMeds. “For example, CoverMyMeds’ central fill facility enables capacity relief and disaster recovery services that give pharmacies alternate prescription fulfillment options in the event they’re at capacity or unable to fill prescriptions at a particular location.”
CoverMyMeds also offers a paperless automated packing device that bundles prescriptions for distribution from a central fill facility to retail stores to help reduce paperwork and costs.
“Additionally, CoverMyMeds continues to find ways to help automate repetitive, time-consuming processes so retail pharmacists can spend more time delivering patient care,” Christie said. “This includes in-workflow technology that automatically compares various cash discount cards in real-time to benefit both pharmacists and patients.”
DrFirst
Founded in 2000, healthcare IT pioneer DrFirst has empowered providers and patients to achieve better health through intelligent medication management, improving healthcare efficiency and effectiveness by enhancing e-prescribing workflows and medication history, optimizing clinical data usability and helping patients start and stay on therapy.
The Rockville, Md.-based company works with more than 325,000 healthcare professionals, including more than 220,000 prescribers in hospitals, clinics and private practices throughout the U.S. and Canada, connecting with over 70,000 pharmacies and integrating with 50% of electronic health record and health information systems.
Two of DrFirst’s AI-powered innovations were recognized by the Edison Awards: SmartSuite for Pharmacy in 2022 and its newest solution, SmartRenewal, in 2023. SmartRenewal bridges the interoperability gap so clinicians can renew prescriptions safely and quickly with fewer manual clicks and keystrokes.
“We have great respect for the role of pharmacists in patient care and are committed to helping them with innovative and intelligent solutions,” said G. Cameron Deemer, CEO of DrFirst. “SmartSuite for Pharmacy by DrFirst uses our patented AI to help process electronic prescriptions faster and safer, saving manual keystrokes that contribute to clinician burnout and errors. We are honored to receive this recognition by Drug Store News for our innovation that makes a difference for pharmacies, pharmacists and patients.”
EnlivenHealth
“From financial solutions and data analytics to patient engagement solutions and software designed specifically to support clinical services, EnlivenHealth provides the technology pharmacists need to operate at the top of their license and best serve their communities,” said Jason Ausili, head of pharmacy transformation at EnlivenHealth.
Launched by parent company Omnicell in October 2020, Fort Worth, Texas-based EnlivenHealth provides more than 50,000 pharmacies across the country with software solutions and technology designed to improve the health of both their patients and their businesses.
“With the acquisition of established pharmacy software providers FDS Amplicare and MarkeTouch Media in 2021, EnlivenHealth now offers the most comprehensive suite of pharmacy software-as-a-service solutions on the market,” Ausili said.
EnlivenHealth’s most recent innovation is Personalized IVR. This interactive voice response solution helps pharmacy staff better utilize their time while enabling patients to get the help they need quickly and efficiently. When a patient calls the pharmacy, the automated phone system identifies them by their phone number, then offers personalized options to refill prescriptions, get medication status updates and check for basic pharmacy information 24 hours a day without interrupting pharmacy staff. “Personalized IVR makes the pharmacy more accessible for patients and it gives pharmacists time back in their day,” Ausili said.
iA
iA, (Innovation Associates), in Indianapolis, is a pharmacy fulfillment company that provides an integrated platform of capabilities to support centralized and community pharmacy solutions.
With more than 30 years of experience in the pharmacy fulfillment business, iA has developed and implemented a suite of automation and software solutions that help deliver quick and sustainable business results. iA’s Pharmacy Fulfillment Platform and people work together to improve customers’ workflow, increase efficiency and optimize fulfillment.
iA continues to tap into its inventive philosophies and develop partnerships that, above all, will drive innovation.
As one of the providers of centralized fulfillment automation, iA’s primary goal is to work with customers and provide a comprehensive solution by utilizing proprietary hardware and intelligent pharmacy fulfillment software, NEXiA. iA’s software helps give pharmacists oversight across every stage of the fulfillment process to support improved workflows, increased efficiencies, reduced fulfillment burdens and lower fill cost.
From the relationships between pharmacists and patients to the trust built with customers, iA’s strong partnerships are integral to everything they do. iA works with pharmacy providers in the commercial, health systems, government and mail order/e-commerce markets.
InStep Health
For over 20 years, Chicago-based InStep Health has offered a platform that connects pharma, OTC and CPG branded messaging with targeted consumers/patients and healthcare providers in meaningful ways at each critical point in the healthcare experience.
InStep Health’s solutions include inStore media activations like static and digital Media Displays on-shelf in the retail aisle, Professional Education Kits for pharmacists and providers in-office and connected measurement data analysis services through its inSights program.
In 2022, InStep Health announced the launch of a new Patient WiFi solution. The offering features software that enables health and wellness brands to connect their message with targeted patients and visitors in more than 60,000 office locations nationwide while they wait for their doctors’ appointments. It’s the ultimate in pre-visit influence. Previously, the company launched its digital Navigator Ad offering, which combines the reach and frequency of digital display advertising with the utility of an HCP provider directory. Based on the patient’s location and likely health condition, the Navigator Ads dynamically generate provider listings that directly offer click-to-call or other real-time appointment booking options within the ad unit.
InStep Health delivers health education via digital and in-person experiences to those making vital healthcare decisions at critical points in the care journey. Pairing the power of tactile and digital media activations with the Connected Messaging Platform, healthcare marketers access more than 250,000 healthcare providers, working in more than 175,000 offices and programs in 42,000 retail and independent pharmacy locations nationwide.
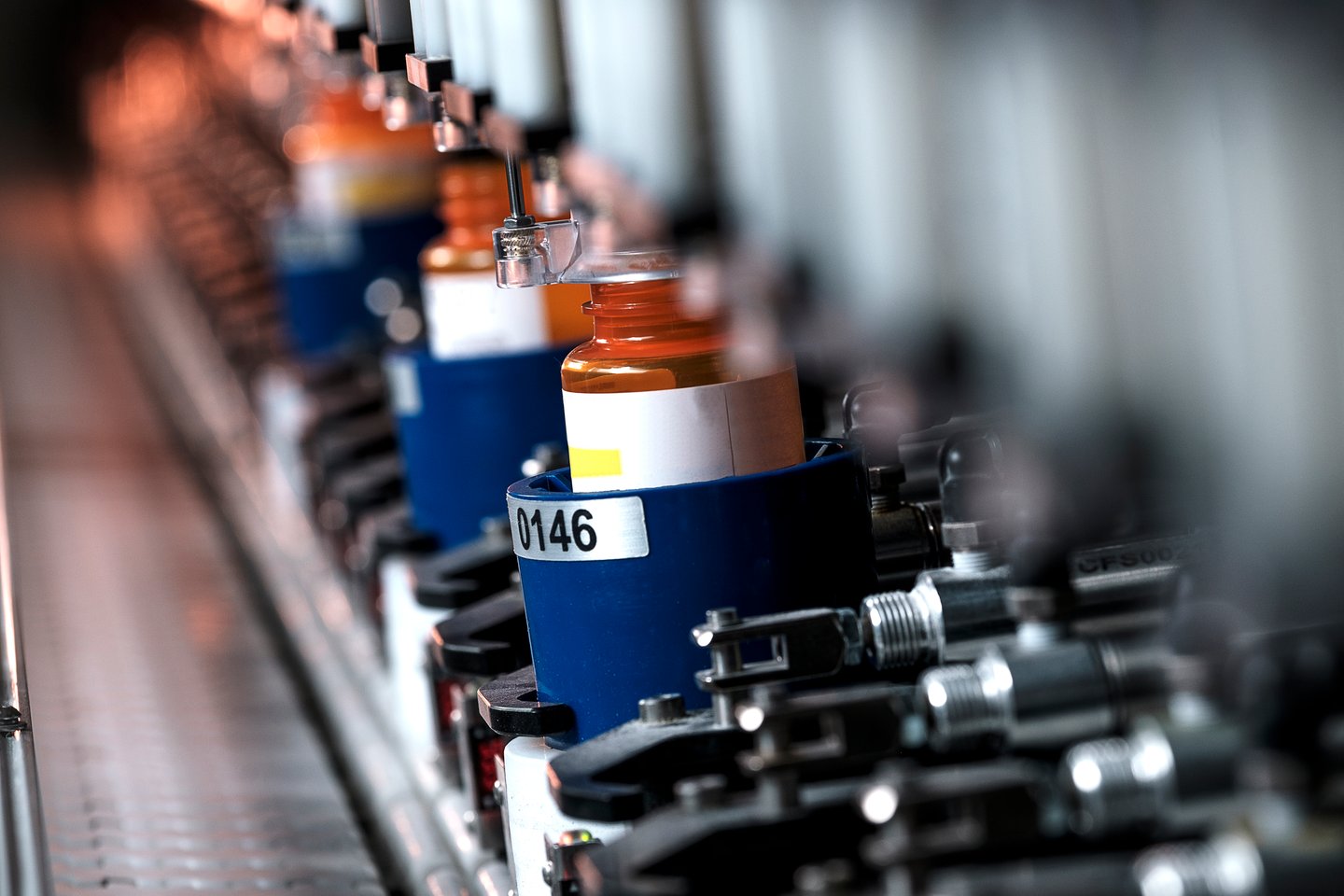
KNAPP
Kennesaw, Ga.-based KNAPP is a global technology company with its North American headquarters in Atlanta.
“For over 40 years, KNAPP has been successfully automating pharmacy operations with our oldest central fill and mail pharmacies still running and expanding over 20 years later. Our unique solutions power some of the biggest names in pharmacy,” said Brian Sullivan, principal of pharmacy solutions at KNAPP North America. “Known as the most durable and reliable systems available, KNAPP has installations in over 1,200 retail pharmacies. We are the only provider of automated grocery and pharmacy BOPIS 24/7 solutions. The largest long term care pharmacies in North America are powered by KNAPP and our specialty pharmacy solutions are changing how medications are fulfilled.”
KNAPP has taken in-store pharmacy automation to the next level with recent installations of its 24/7 terminals. Fully automated dispensing of will-call orders is now available in-store and at the drive-thru at any time of day. Unlike locker systems, store personnel can provide these orders without additional effort.
“Integral telepharmacy capabilities provide patients access to acute medications when they need it. Additionally, the automated put away of stock provides the pharmacy additional time savings and automated DSCSA scanning to stay ahead of upcoming requirements,” Sullivan said.
LexisNexis Risk Solutions
Serving customers across the retail pharmacy, specialty pharmacy, PBM, payer, provider, life sciences and health IT markets, the healthcare business of LexisNexis Risk Solutions better enables organizations to solve a range of challenges, such as patient engagement, identity access management, data de-identification, linking and compliance.
Headquartered in Alpharetta, Ga., LexisNexis Risk Solutions addresses these challenges by leveraging consumer, medical claims, provider and social determinants of health data to deliver insights that can improve patient outcomes, support more efficient business operations and create healthier communities, the company said
“LexisNexis VerifyRX is a real-time, compliance-driven prescriber verification solution, designed specifically for retail pharmacy and specialty pharmacies,” said Craig Ford, vice president of sales for pharmacy, healthcare business at LexisNexis Risk Solutions.
As part of the pharmacy workflow, VerifyRX processes millions of transactions a day, verifying complex prescriber data, including Drug Enforcement Administration and state data (when available) and daily National Technical Information Service data.
“Today VerifyRX offers VerifyRX Accelerate, an even more flexible tool that allows users to create additional compliance checks that are unique to their own needs,” Ford said. “This solution not only helps mitigate compliance risk, but also identifies potential claims submission errors prior to dispensing the drug. It also helps pharmacy providers increase the percentage of paid prescription claims.”
Manrex
“Recognition of Manrex by Drug Store News with a REX award in the pharmacy technology/automation category, for the second year, is incredibly exciting and gratifying. We believe this nomination reflects our mission of ensuring our products and services are always directed, first and foremost, towards helping independent pharmacists improve their care model efficiency, while offering outstanding medication safety to their customers,” said John Webster, vice president of innovation and product development at Manrex.
Winnipeg, Canada-based Manrex’s focus on matching the pharmacy automation to the size, strategy and capabilities of the individual pharmacy ensures that the solution not only improves their business but helps them maximize their customer relationships.
Manrex’s RM1 vision-based pill counter, which is sold in the United States by Crocus Medical, is “an inexpensive, entry level pill counter that counts pills in seconds, at a very low price, and is a fantastic way for an independent pharmacy to cut down dispensing times,” Webster said. “Perfect for quick dispensing counts, narcotic counts (double counts in seconds) and inventory counts of any open bottle all without calibration, bar code scanning or interfacing…the inexpensive RM1 is simple, fast and accurate.”
McKesson
As a diversified healthcare services leader, Irving, Texas-based McKesson is committed to helping strengthen the overall health of pharmacies and elevate their role in people’s lives.
“We are working to advance reliable product access and fulfillment, and deliver scalable healthcare solutions, which help pharmacists practice at the top of their license,” said Scott Kemme, senior vice president of pharmaceutical technology and innovation at McKesson.
Whether it’s offering upgrades to their inventory management system or using AI to streamline workflow, McKesson provides pharmacies across care settings with innovative, practical solutions to help improve clinical performance and business operations and expand capabilities to meet the evolving needs of today’s pharmacy customers.
McKesson’s clinically driven pharmacy solutions help customers start their business through its EnterpriseRx pharmacy management software, run their business through patient engagement and clinical services and expand business through pharmacy optimization offerings.
Most recently, McKesson introduced Central Fill as a Service that allows pharmacies to use central fill without the investment in equipment, inventory or staffing. McKesson also recently launched Pinpoint Community Solutions, a perpetual inventory management system designed for independent pharmacies.
“Supporting pharmacies and finding new ways to help them improve the care they deliver while reducing costs and improving efficiency continues to be a focus for McKesson,” Kemme said.
OmniSYS
Dallas-based OmniSYS is a technology company with 25 years of experience working with pharmacies, payers, providers and pharmaceutical manufacturers. As a trusted advisor, OmniSYS serves 50% of U.S. retail pharmacies. Using its unique insight and pharmacy workflow expertise, OmniSYS develops advanced technology solutions that increase efficiency, enabling pharmacies to deliver clinical services that improve patient health and pharmacy business.
“Pharmacies are becoming the chosen source of first-line care for patients, and we’re proud to offer the technology solutions needed to maximize pharmacies’ capabilities and efficiencies to provide more healthcare services to the communities they serve,” said David Pope, chief pharmacy officer at OmniSYS.
Pope pointed out that pharmacies can expand their services more than ever. However, many struggle to deliver clinical services without the help of technology. “From clinical documentation and patient engagement to medical billing, we offer purpose-built, pharmacy-first solutions that provide the interoperability and simplicity needed to optimize patient care, workflow and profitability,” Pope said.
OmniSYS offers the pharmacy industry’s first electronic cloud-based, billing-enabled EHR, bringing together pharmacy and medical information into an insightful patient record that empowers pharmacists to deliver and document clinical services.
OmniSYS’s cloud-based patient engagement solution empowers pharmacies to communicate better with patients. The platform is built on deep clinical intelligence and consumer preferences. It delivers timely, personalized messaging via text, web, mobile and IVR, enhancing the experience, improving adherence and building satisfaction and loyalty.
To help pharmacies bill for clinical services, OmniSYS offers the industry’s leading medical claims billing solution trusted by more than 30,000 pharmacies. With this solution, pharmacies can bill and get paid for immunizations, clinical services, DME and specialty medications.
ScriptPro
Twenty-five years ago, the first ScriptPro robots were delivered to customers—robots that are still filling prescriptions today. This level of longevity provides tremendous value to customers and makes the company unique in the industry, not to mention the unparalleled reliability and sound return on investment.
The staying power of ScriptPro’s robotic systems has been a key driver in ScriptPro creating an ever-expanding platform that now includes powerful pharmacy software, clinical programs, financial management tools and beyond. One of ScriptPro’s latest inventions is the Storage and Retrieval System, a fully automated will-call robot. And, with more patient populations seeing the adherence benefits of their medications being offered in daily packs, the company launched a medication pouch packaging solution.
ScriptPro’s integrated solutions meet the needs of the full range of pharmacies of any scale and across all healthcare settings. The platform replaces a collection of applications that are otherwise required to get the job done.
ScriptPro continues to create and provide relevant, powerful tools to help pharmacies continually offer world-class pharmacy services to their patients and communities.
STChealth
Headquartered in Phoenix, STChealth works with clients throughout the United States and internationally to pursue a shared mission of eradicating vaccine-preventable disease through innovative software and service solutions.
More than 80,000 immunization providers located across all 50 U.S. states leverage STChealth clinical services technology to validate patient immunization status, as well as to capture and report patient immunization and laboratory test data to state and federal entities. Since the outset of the COVID pandemic, more than 1 billion patient records have been reported through STChealth’s national provider network. This massive exchange of data was made possible through partnerships with The White House, the Centers for Disease Control and Prevention, state public health and community pharmacies across the nation.
“Throughout its history, STChealth has worked alongside public health as a provider of immunization information system technology,” said Mike Popovich, CEO of STChealth. “These public sector relationships allow STChealth to bridge the gap with private sector healthcare providers, including pharmacy, to create longstanding and meaningful partnerships between immunization providers and public health organizations. While many in the healthcare ecosystem recognize the risk that vaccine hesitancy poses to public health, few are taking action like STChealth. Leveraging the billions of data points that run through STChealth systems, ongoing research and development is underway to help immunization providers make better decisions about enabling access, in addition to helping providers determine when and how to communicate with vaccine hesitant patients.”
Surescripts
Arlington, Va.-based Surescripts has transformed healthcare interoperability in the two decades since first enabling electronic prescribing nationwide in 2001. Surescripts continues bringing greater clarity and efficiency to prescriber/pharmacist communication while increasing patient safety in the 2.34 billion e-prescriptions the network supported in 2022.
“Surescripts is simplifying health intelligence sharing, delivering the right clinical information at the right time,” said Lawrence King, director of product safety and performance at Surescripts, noting that more than two million providers exchanged patient data more than 21 billion times, supporting better informed and less costly care.
Surescripts Real-Time Prescription Benefit gives clinicians actionable information about a patient’s prescription drug benefit at the time of prescribing and at the pharmacy, saving patients an average of $61 on traditional prescriptions and $428 on specialty medications.
“Surescripts technology is empowering pharmacists to do more than fill prescriptions, enabling them to do what they do best: provide comprehensive, accessible care as part of a patient’s care team,” King said. “Advancing healthcare interoperability combined with Surescripts technology is helping to reduce burnout-causing administrative tasks for pharmacists and physicians. Surescripts Specialty Medications Gateway is allowing pharmacists to access key patient information from the EHR so they spend less time calling and faxing providers to obtain missing information. With 20 million specialty prescriptions processed electronically last year, the Surescripts Network Alliance is working to help patients start their medications sooner, and helping their care teams spend less time on administrative tasks.”